PAIN MANAGEMENT MEDICAL BILLING
BILLING AND CODING SERVICES
Pain Management Billing Services:
Pain management specialists deal with patients who are suffering, and they know how important treatment is—but payers are often extremely critical of billing for pain treatment when the cause isn’t something that shows up on an x-ray or has a disease diagnosis. Recent regulations have increased scrutiny of medications used for pain and the penalties for misuse to the extent that many doctors refuse to practice pain management.
Pain Management Coding and Billing Errors
With these inherent hurdles to deal with, it becomes even more important that practitioners aren’t burdened by Pain Management billing issues. Across all fields of medicine, institutions are cutting costs and payers are looking for ways to reduce what they pay, including being very particular about billing and coding errors, which result in claims being rejected or denied.
Billing Challenges for Pain Management Centers & Practitioners
It’s possible for Pain Management Centers to offer fewer pain management services as compared with other health care providers because more than 100 million Americans experience chronic pain. An examination of the most common issues in pain management billing services revealed these common challenges.
Claim Denial Management
Rejection or denial of claims for the tiniest errors is common. Every letter must match the patient record exactly, and payers do not even try to determine what was meant if something seems amiss. The pain management billing RCM process relates to every aspect of patient care from patient intake information to payment collection, so there are innumerable errors that can be made in entering just the right information.


Administrative Delays
Many pain management practices manage claim denials by a very laborious manual process done by in-house staff. This results in slow claim submission and increased labor costs. Outsourcing pain management billing services to a team of specialists can significantly improve claim denial resolutions, case mix performance and the time claims are in accounts receivable.
Increased Financial Responsibility of Patients:
An analysis conducted by Trans Union Healthcare in 2017 found that patients’ healthcare providers costs had increased by up to 11%. Rapidly increasing patient costs mean it is more important than ever to fully inform patients about their financial responsibility prior to treatment. The increased costs are also making it more difficult for pain management practices to collect the amount due to them.

The Solution to Pain Management Billing Issues
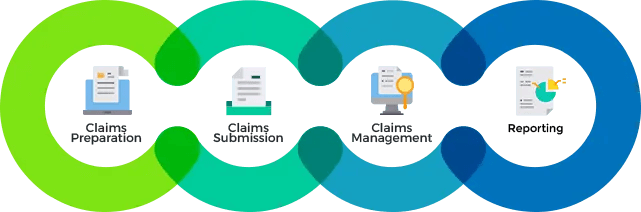
Med Bridge takes care of revenue cycle management (RCM) from beginning to end, allowing pain management doctors and staff to focus on patients, knowing that the necessary billing and coding services are getting done. The extent of services includes not only what would be assumed to be part of Pain Management medical billing, but also payroll costs, revenue increments, ensuring compliance and more.
Focus On Patient Care
Outsourcing medical billing should not be seen as a cost burden for your practice management, but as a service that will free up practitioners and staff to focus on patients, while increasing revenue by efficiently filing claims, managing rejections, and denials, and avoiding up coding and down coding errors. We even take care of annual payer adjustments, completing the cycle as revenue cycle management.
Run Practice More Efficiently
As specialists in medical billing and coding, Med Bridge keeps up with the annual code changes as well as the various rules and pain management billing guidelines that are constantly changing. Because we have customers of all sizes, in every major field of medicine, or certified coders are kept up to date and trained on the specialized codes of each specialty they work with. Get a free demo today and see how we can help you and your practice run more efficiently, increase revenue & improve cash flow.
